about fibromyalgia
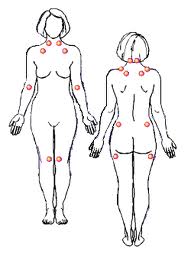
Fibromyalgia is an increasingly recognized chronic pain illness which is characterized by widespread musculoskeletal aches, pain and stiffness, soft tissue tenderness, general fatigue and sleep disturbances. The most common sites of pain include the neck, back, shoulders, pelvic girdle and hands, but any body part can be involved. Fibromyalgia patients experience a range of symptoms of varying intensities that wax and wane over time.
It is estimated that approximately 3-6% of the U.S. population has Fibromyalgia. Although a higher percentage of women are affected, it does strike men, women and children of all ages and races. Because of its debilitating nature, Fibromyalgia has a serious impact on patients' family, friends, and employers, as well as society at large.
Fibromyalgia is characterized by the presence of multiple tender points and a constellation of symptoms. The pain of Fibromyalgia is profound, widespread and chronic. It knows no boundaries, migrating to all parts of the body and varying in intensity. Fibromyalgia pain has been described as deep muscular aching, throbbing, twitching, stabbing and shooting pain that defines the very existence of the Fibromyalgia patient. Neurological complaints such as numbness, tingling and burning are often present and add to the discomfort of the patient. The severity of the pain and stiffness is often worse in the morning. Aggravating factors which affect pain include cold/humid weather, non-restorative sleep, physical and mental fatigue, excessive physical activity, physical inactivity, anxiety and stress.
Fatigue
In today's world many people complain of fatigue; however, the fatigue of Fibromyalgia is much more than being tired. It is an all-encompassing exhaustion that interferes with even the simplest daily activities. It feels like every drop of energy has been drained from the body, which at times can leave the patient with a limited ability to function both mentally and physically.
Sleep Problems
Many Fibromyalgia patients have an associated sleep disorder which prevents them from getting deep, restful, restorative sleep. Medical researchers have documented specific and distinctive abnormalities in the stage 4 deep sleep of Fibromyalgia patients. During sleep, individuals with Fibromyalgia are constantly interrupted by bursts of awake-like brain activity, limiting the amount of time they spend in deep sleep.
Additional symptoms may include: irritable bowel and bladder, headaches and migraines, restless legs syndrome (periodic limb movement disorder), impaired memory and concentration, skin sensitivities and rashes, dry eyes and mouth, anxiety, depression, ringing in the ears, dizziness, vision problems, raynaud's syndrome, neurological symptoms and impaired coordination.
Currently there are no laboratory tests available for diagnosing Fibromyalgia. Doctors must rely on patient histories, self-reported symptoms, a physical examination and an accurate manual tender point examination. This exam is based on the standardized ACR criteria. Proper implementation of the exam determines the presence of multiple tender points at characteristic locations.
It is estimated that it takes an average of five years for a Fibromyalgia patient to get an accurate diagnosis. Many doctors are still not adequately informed or educated about Fibromyalgia. Laboratory tests often prove negative and many Fibromyalgia symptoms overlap with the symptoms of other conditions, thus leading to extensive investigative costs and frustration for both the doctor and patient. Another essential point that must be considered is that the presence of other diseases, such as rheumatoid arthritis or lupus, does not rule out a Fibromyalgia diagnosis. Fibromyalgia is not a diagnosis of exclusion and must be diagnosed by its own characteristic features. To receive a diagnosis of Fibromyalgia, the patient must meet the following diagnostic criteria:
Widespread pain in all four quadrants of the body for a minimum duration of three months Tenderness or pain in at least 11 of the 18 specified tender points when pressure is applied
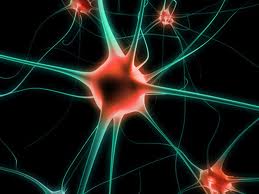
While the underlying cause or causes of Fibromyalgia still remain a mystery, new research findings continue to bring us closer to understanding the basic mechanisms of Fibromyalgia. Most researchers agree that Fibromyalgia is a disorder of central processing with neuroendocrine/neurotransmitter dysregulation. The Fibromyalgia patient experiences pain amplification due to abnormal sensory processing in the central nervous system. An increasing number of scientific studies now show multiple physiological abnormalities in the Fibromyalgia patient, including: increased levels of substance P in the spinal cord, low levels of blood flow to the thalamus region of the brain, HPA axis hypofunction, low levels of serotonin and tryptophan and abnormalities in cytokine function.
Recent studies show that genetic factors may predispose individuals to a genetic susceptibility to Fibromyalgia. For some, the onset of Fibromyalgia is slow; however, in a large percentage of patients the onset is triggered by an illness or injury that causes trauma to the body. These events may act to incite an undetected physiological problem already present.
Exciting new research has also begun in the areas of brain imaging and neurosurgery. Continued work will look at the hypothesis that Fibromyalgia is caused by an interpretative defect in the central nervous system that brings about abnormal pain perception. Medical researchers have just begun to untangle the truths about this life-altering disease.
One of the most important factors in improving the symptoms of Fibromyalgia is for the patient to recognize the need for lifestyle adaptation. Most people are resistant to change because it implies adjustment, discomfort and effort. However, in the case of Fibromyalgia, change can bring about recognizable improvement in function and quality of life. Becoming educated about Fibromyalgia gives the patient more potential for improvement.
An empathetic physician who is knowledgeable about the diagnosis and treatment of Fibromyalgia and who will listen to and work with the patient is an important component of treatment. It may be a family practitioner, an internist or a specialist (rheumatologist or neurologist, for example). Conventional medical intervention may be only part of a potential treatment program. Alternative treatments, nutrition, relaxation techniques and exercise play an important role in Fibromyalgia treatment as well. Each patient should, along with the healthcare practitioner, establish a multifaceted and individualized approach that works for them.
Pain Management
Over-the-counter pain medications, such as acetaminophen or ibuprofen, may be helpful in relieving pain. The physician may decide to prescribe one of the newer non-narcotic pain relievers (e.g. tramadol) or low doses of antidepressants (e.g. tricyclic antidepressants, serotonin reuptake inhibitors) or benzodiazepines. Patients must remember that antidepressants are "serotonin builders" and can be prescribed at low levels to help improve sleep and relieve pain. If the patient is experiencing depression, higher levels of these or other medications may need to be prescribed. Another beneficial pain therapy, which works well on localized areas of pain, is lidocaine injections into the patient's tender points. An important aspect of pain management is a regular program of gentle exercise and stretching, which helps maintain muscle tone and reduces pain and stiffness.
Sleep Management
Improved sleep can be obtained by implementing a healthy sleep regimen, which includes going to bed and getting up at the same time every day, making sure that the sleeping environment is conducive to sleep (i.e. quiet, free from distractions, a comfortable room temperature, a supportive bed), avoiding caffeine, sugar and alcohol before bed, doing some type of light exercise during the day, avoiding eating immediately before bedtime and practicing relaxation exercises as you fall to sleep. When necessary, there are new sleep medications that can be prescribed, some of which can be especially helpful if the patient's sleep is disturbed by restless legs or periodic limb movement disorder.
Psychological Support
Learning to live with a chronic illness often challenges an individual emotionally. The Fibromyalgia patient needs to develop a program that provides emotional support and increases communication with family and friends. Many communities throughout the United States and abroad have organized Fibromyalgia support groups. These groups often provide important information and have guest speakers who discuss subjects of particular interest to the Fibromyalgia patient. Counseling sessions with a trained professional may help improve communication and understanding about the illness and help to build healthier relationships within the patient's family.
Other Treatments
Complementary therapies can be very beneficial. These include: physical therapy, therapeutic massage, myofascial release therapy, water therapy, light aerobics, acupressure, application of heat or cold, acupuncture, yoga, relaxation exercises, breathing techniques, aromatherapy, cognitive therapy, biofeedback, herbs, nutritional supplements, and osteopathic or chiropractic manipulation. What is the prognosis? Better than ever before! The efforts of individuals, support groups, organizations and medical professionals to help improve the quality of life for people with Fibromyalgia are starting to pay off. Better ways to diagnose and treat Fibromyalgia are on the horizon. The symptoms of Fibromyalgia can vary in severity and often wax and wane, but most patients do tend to improve over time. By actively seeking new information, talking to others who have Fibromyalgia, re-evaluating daily priorities, making lifestyle changes, and working hard to keep a hopeful attitude, the Fibromyalgia sufferer can become the Fibromyalgia survivor!
Source: National Fibromyalgia Association.
Supplements for Fibromyalgia (Woodland Health) by Joe M., Ph.D. Elrod
What Your Doctor May Not Tell You About Fibromyalgia:
The Revolutionary Treatment That Can Reverse the Disease
by R. Paul St. Amand, Claudia Craig Marek
Chronic Fatigue Syndrome (CFS/ME): The Facts
by Frankie Campling, Michael Sharpe
Fibromyalgia and Chronic Fatigue Myofascial Pain: A Survival Manual
by Devin J Starlanyl, Mary Ellen Copeland
The Fibromyalgia Cookbook: More Than 120 Easy and Delicious Recipes by Shelley Ann Smith, Alsion Bested
national fibromyalgia association
medline plus links: fibromyalgia article
fibromyalgia is a medical condition, not a psychological disorder... the pain is not in your head... it is in the myofascial tissue.
Double-click to edit text, or drag to move.